Despite efficiencies imposed elsewhere, the new administration made waves this month with their newly released 2026 proposed Physician Fee Schedule ("PFS") boosting reimbursements for chronic and other care management codes.TL;DR Reimbursements for key chronic disease programs are proposed to increase ~8-10% in 2026. One of the largest increases ever. NOTE: Medicare will also pay 0.5% more for providers participating in qualifying Alternative Payment Model (“APM”).Here’s the break-down (and there's a full code-by-code table below) focusing on the most common care management CPT codes: Chronic Care Management (“CCM”), Remote Therapeutic Monitoring (“RTM”) and Remote Patient Monitoring (RTM + RPM):Chronic Care Management (CCM) The 2026 Medicare Physician Fee Schedule proposes a significant ~9% increase in Chronic Care Management (CCM) reimbursement, with no new codes introduced. The base code for 20 minutes of staff-led care (99490) will see an 8.6% increase, rising from $60.49 to $65.67. The add-on code for each additional 20 minutes (99439) will rise by 9.4%, from $45.93 to $50.26. These reimbursement figures are based on national average payment rates and reflect CMS’s continued investment in longitudinal chronic care, offering providers a boost in revenue for supporting patients with complex conditions.Remote Therapeutic Monitoring (RTM) RTM reimbursement is set to grow significantly in 2026, primarily due to new codes that cover 2–15 days of data collection—unlocking payments for roughly 20% more patients who previously didn’t meet the 16-day threshold. In addition to the new device (98XX5) and treatment management (98XX7) codes, several existing RTM services will see national average payment increases of ~5–10%. For example, code 98980 (first 20 minutes of treatment management) will increase 7.6% to $53.94. The overall effect is a ~20% boost in reimbursable RTM services.Remote Physiologic Monitoring (RPM) RPM services will see a similar ~25% overall increase in reimbursement, also driven by new codes including 99XX4 which pays for less days, 2–15 days, of data submission per 30 day period. These additions make more patients eligible for billing and reduce uncompensated care. Alongside the new codes, existing RPM reimbursements are also rising: 99457 (first 20 minutes of care) increases 8.5% to $51.93, and 99458 (each additional 20 minutes) rises 7.9% to $41.55. These reimbursement amounts reflect national averages and underscore CMS’s growing recognition of the role remote monitoring plays in effective chronic disease management.
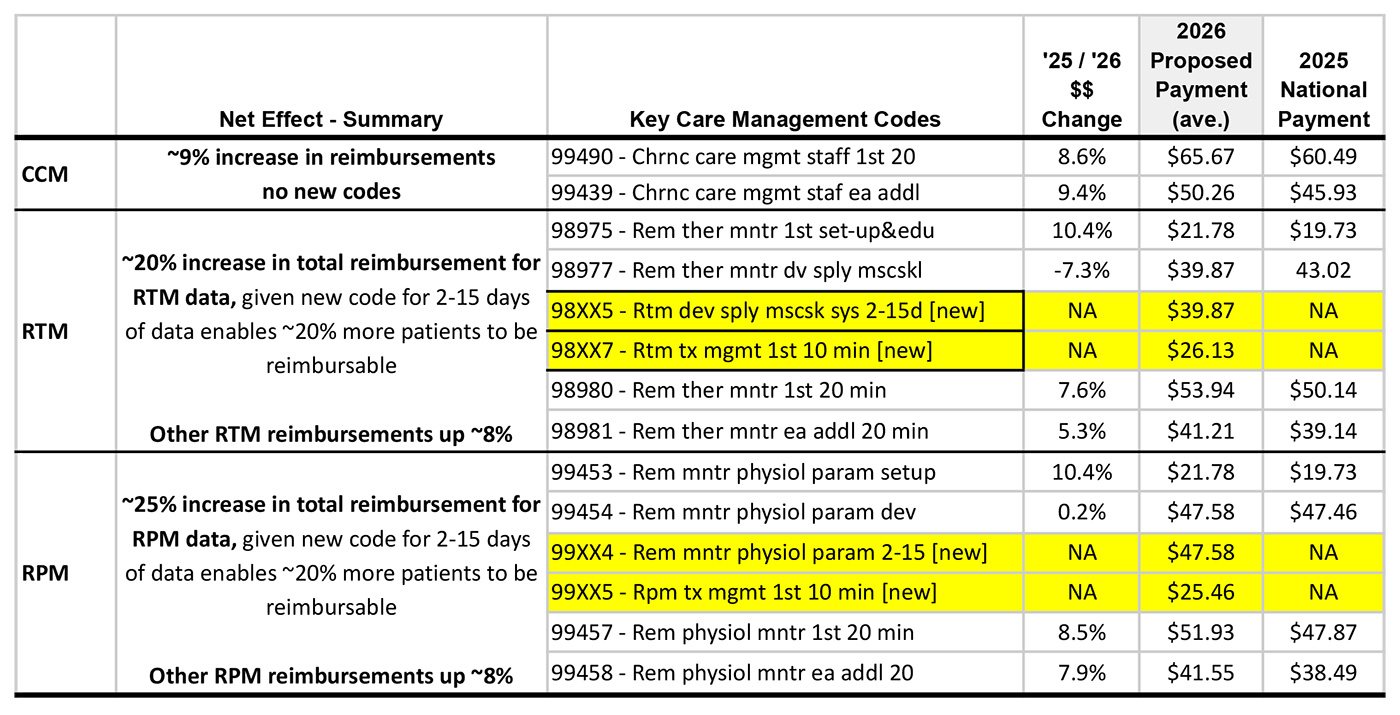
*NOTE: all 2026 reimbursement amounts above are an average of APM and non-APM calculations. The difference between APM and non-APM amounts is small: 0.5%.Bottom line: the 2026 proposed rule is one of the strongest signals yet that CMS is prioritizing chronic care—especially when supported by remote monitoring.Want to leverage these enhanced codes to unlock more care for your patients? Let’s talk.